What is Peroneal Retinaculum
The Peroneal tendons may dislocate and repetitively subluxation from behind the lateral malleolus as a result of trauma in high-end athletes. Now let’s find out how Rupture of the Peroneal Retinaculum occurs and its ultimate treatment.
Epidemiology:
Mostly peroneal subluxation or dislocation occurs in young, active individuals/ athletes.
Mechanism of injury:
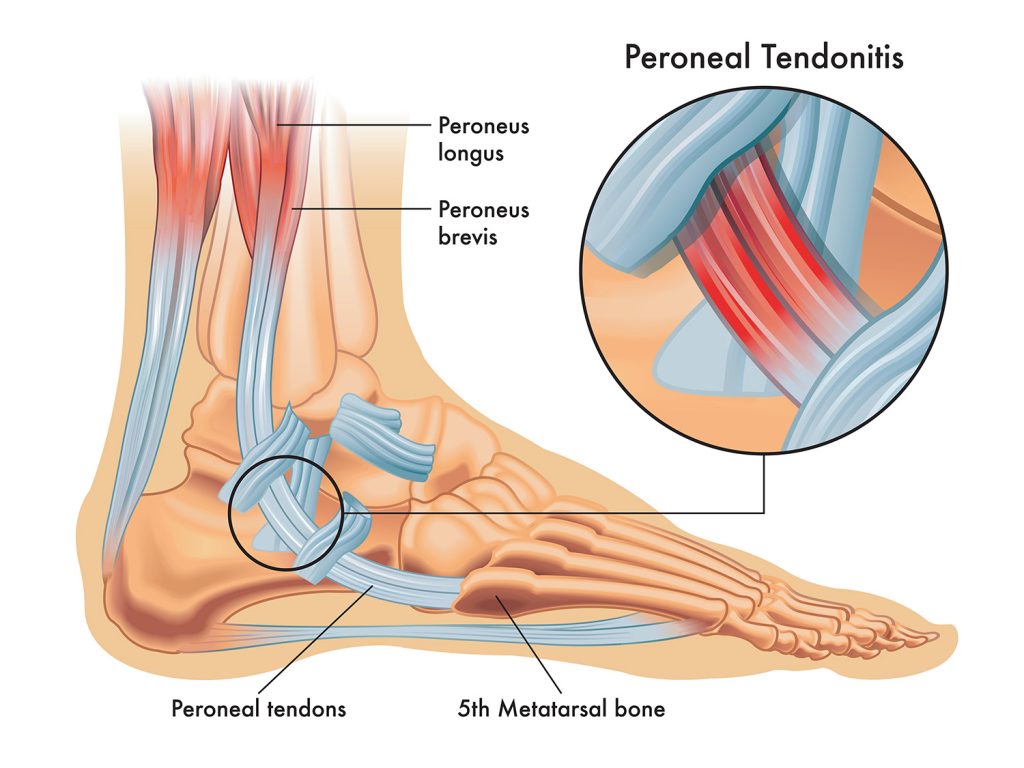
Rapid Dorsiflexion of an inverted foot leading to a rapid reflexive contraction of the peroneus Longus and peroneus Brevis tendons can tear off the peroneal retinaculum causing subluxation/dislocation of the tendons.
Pathophysiology of Peroneal Retinaculum:
Subluxation of the peroneal tendons leads to longitudinal tears over time which usually involves Peroneus Brevis at the fibular groove. Subfibular impingement is seen occurs secondary to calcaneal malunion at the site of torn superior Peroneal Retinaculum, in medical terms which we say rupture of Peroneal Retinaculum.
ASSOCIATED CONDITIONS
This condition may be associated with tears of the Peroneus Brevis and/or Peroneus Longus. The tear is mostly a longitudinal split rather than a transverse split. In up to 75% of such patients, lateral ankle ligament injuries (Anterior Talofibular Ligament, Calcaneofibular ligament) are also seen with superior peroneal retinaculum tear, which can be effectively managed with pain free physiotherapy.
Classification of Peroneal Retinaculum
| Ogden Classification of Superior Peroneal Retinaculum (SPR) Tears | |
|---|---|
| Grade 1 | The SPR is partially elevated off of the fibula allowing for the subluxation of both tendons |
| Grade 2 | The SPR is separated from the cartilage fibrous ridge of the lateral malleolus, allowing the tendons to sublux between the SPR and the cartilage fibrous ridge |
| Grade 3 | There is a cortical avulsion off the SPR off of the fibula, allowing the subluxated tendons to move underneath the cortical fragment |
| Grade 4 | The SPR is torn from the calcaneus, not the fibula. |
Presentation:
The patient often complains of a popping/ snapping feeling with a dorsiflexion and inversion ankle injury. There is clicking, popping or snapping and feelings of instability or pain on the lateral aspect of the ankle.
Swelling can be seen posterior to the lateral malleolus. Tenderness can be elicited over the tendons or posterolateral aspect of the ankle on palpation.
A ‘pseudotumor’ like bulging over the peroneal tendons can be seen. Patients can voluntarily subluxation the tendons with or without a popping sound.
Provocative/ Special Test:
- Apprehension tests
The sensation of apprehension or subluxation with active dorsiflexion and eversion against resistance causes subluxation/dislocation with apprehension.
- Compression test
Pain/ apprehension with passive dorsiflexion and eversion of the ankle in patients with superior peroneal retinacular tear.
Imaging:
A plain x-ray in an internally rotated view will show a cortical avulsion off the distal tip of the lateral malleolus (fleck sign, rim fracture). The patient should be evaluated for varus hindfoot deformity.
MRI – An axial view of a slightly flexed ankle can demonstrate anatomic anomalies leading to pathologies such as an additional peroneus Quartus muscle or a low-lying peroneus brevis muscle belly.
Treatment Of Rupture of Peroneal Retinaculum
 Non-operative: Short leg cast immobilization and protected weight-bearing for 6 weeks
Non-operative: Short leg cast immobilization and protected weight-bearing for 6 weeks
- Indications – all acute injuries in nonprofessional athletes
- Technique – tendons of peroneal muscles are reduces reduced at the time of applying the cast.
- Outcomes – success rates for nonsurgical management are only marginally better than 50%.
- Operative:
- Acute repair of superior peroneal retinaculum and deepening of the fibular groove
Indications – Acute Tendon Dislocations in serious athletes who desire a quick return to sports or individuals with an active lifestyle – the presence of a longitudinal tear
- Groove-deepening with soft tissue transfer and/or osteotomy
Indications – Chronic/Recurrent Dislocation
Technique: If reconstruction of the Superior Peroneal Retinaculum Tear is not possible, treatment focuses on other aspects of peroneal stability typically involves groove-deepening in addition to soft tissue transfers or bone block techniques (osteotomies to further contain the tendons within the sulcus)
Grafting the Plantaris muscle can be done to reinforce the superior peroneal retinaculum.
The hindfoot varus must be corrected prior to any SPR reconstructive procedure.






 Non-operative: Short leg cast immobilization and protected weight-bearing for 6 weeks
Non-operative: Short leg cast immobilization and protected weight-bearing for 6 weeks