What is Osteochondritis Dissecans of Talus?
Osteochondritis dissecans of Talus (OCD) is a condition that develops in joints, most often in children and adolescents. It occurs when a small segment of bone begins to separate from its surrounding region due to a lack of blood supply. As a result, the small piece of bone and the cartilage covering it begin to crack and loosen.
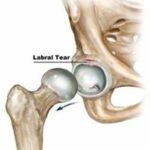
Osteochondritis dissecans of the talus is defined as a subchondral bony lesion of a small fragment of bone, usually less than 2 cm in diameter, with overlying intact articular cartilage. This fragment then becomes separated from its bed and undergoes necrosis. Earlier researchers described the lesion as being traumatic in origin but revised their opinion towards that of an “avascular” process. To add to the confusion there are a number of synonyms for this lesion: Osteocartilaginous body, joint mice, loose bodies, intra-articular fragmentary fracture, and transchondral fracture of the talus. Earlier controversies about etiology centered on disputes between traumatic and vascular factors. Those who feel that it is a traumatic lesion refer to it as a transchondral fracture of the talus or transchondral talar dome fractures.
Mechanism of injury
The injury is sustained during the inversion of the ankle. If the foot is plantarflexed during inversion, a medial lesion will result from compression of the medial talar dome by the tibia, secondary to spiraling and shortening of the collateral ligaments. If the foot is dorsiflexed, a lateral lesion will result from shearing forces by the fibula. The anatomy of the talar dome and the ankle mortise is such that medial lesions are posterior and lateral lesions more anterior.
Symptoms of Osteochondritis Dissecans of Talus?
The symptoms of Osteochondritis dissecans of the talus can be either acute or chronic. With an acute injury, the symptoms will be of the initial trauma (usually an inversion injury), which will predominate with eventual resolution in three to six weeks, followed by the onset of chronic symptoms. A chronic condition may or may not have a history of injury primarily, with symptoms of pain, stiffness, instability, or locking.
Classification of OCD by Berndt and Harty
Stage 1. A small area of compression of the subchondral bone
Stage 2. Partially detached Osteochondral fragment (flap)
Stage 3. Completely detached Osteochondral fragment but undisplaced
Stage 4. Free Osteochondral fragment
Diagnosis
X-ray CT scan or an MRI is commonly used for the diagnosis of the condition.
Treatment of Osteochondritis Dissecans of Talus?
- Conservative Treatment
Treatment of OCD is guided by the patient’s age at the onset of symptoms, their severity, and the disease stage according to the Berndt and Harty classification. OCD can remain asymptomatic throughout a patient’s life, or it can become symptomatic as a result of a trauma, even in adulthood.
In most cases discovered during adolescence, the overlying cartilage layer is completely intact (stage I). Stage I and stage II lesions in teenagers are usually treated conservatively. For stage I lesions, treatment consists of leg cast immobilization and protected weight-bearing on the affected ankle for six weeks. Physical activity is limited for at least six months. In stage II lesions, weight-bearing is prohibited for six weeks. This period is followed by two weeks of partial weight-bearing.
- Surgical Treatment
Indications for surgery are stage III or IV lesion, failure of conservative treatment, detachment of the fragment, or decreased potential for revascularization.
Surgery usually involves removing the loose fragment of cartilage and bone from the ankle joint and drilling small holes in the injured bone. When the fragment is removed, a defect shaped like a small crater is left in the talar dome. It is this area where the drill holes are made. The drill holes allow new blood vessels to grow into the defect and help to form scar tissue to fill the area. Eventually, this new scar tissue smoothes out the defect and allows the ankle to move more easily.
- Arthroscopic Method
In some cases, the surgery may be done using an arthroscope. An arthroscope is a special miniature TV camera that is inserted into the joint through a very small incision. Special instruments are inserted into the ankle through other small incisions. By watching on the TV screen, the surgeon removes the fragment and drills the defect.
- Open Method
The ankle is a small joint, so it is sometimes difficult to get the arthroscope into certain areas. If the defect is in an area of the ankle difficult to reach with the arthroscope, an open incision may be required. This incision is usually made in the front of the ankle to allow the surgeon to see into the joint. Special instruments are used to remove the fragment and drill the injured area.
- Post-surgical Rehabilitation
Patients normally require crutches to prevent bearing weight on the ankle for four to six weeks after surgery. A bandage or dressing is applied for a week following the surgical procedure. The stitches are generally removed in 10 to 14 days. However, if the surgeon used sutures that dissolve stitches are not required to be removed.
Active range of motion exercises is started very soon after surgery. Patients wear a splint that can easily be removed to do the exercises throughout the day.
The physiotherapist will initially aim to control the pain and swelling post-surgery. As a part of injury protection physiotherapist will make the patient learn how much weight to be kept on the operated leg.
Gradual strengthening exercises are implemented in a safe position of the ankle to avoid any damage to healing tissues. Complete leg strengthening exercises with core strengthening should be taught to the patient. Once complete weight-bearing is started patient can be progressed through proprioceptive exercises, cycling, and other challenging/ demanding exercises like speed, agility, and endurance exercises.